Oxalates in Food: 8 GAPS, AIP, and Paleo Approved Foods that Contribute to Hashimoto's, Arthritis, and More
Imagine you are a leaf of spinach. Would you like to be eaten? Probably not. And for this reason you have protective parts that develop in your biology called oxalates or oxalic acid. These are meant to deter your predators (i.e. humans and other animals) from eating all of you and they succeed. Some people who over consume these plant toxins develop diseases and health complications. The plant species ultimately wins the war, even if it lost the battle and was eaten.
As a functional nutritionist in practice over the last 9 years, I’ve come to appreciate and respect plant toxins such as oxalates. In fact, oxalates contributed to my own chronic illness for many years without my knowledge. Understanding the effects of oxalic acid on the human body enabled me and has allowed many of my clients to overcome the last hurdles in our healing journeys.
This article will equip you to decipher if you have over consumed oxalates and how to protect yourself from this plant toxin without fearing food.
What are Oxalates
Oxalates or oxalic acid are plant toxins similar to those known as phytates, lectins, goitrogens, and tannins. The molecular makeup of this particular toxin makes it water-soluble, meaning it is easily absorbed. It is crystal-like and can bind to positively charged ions like calcium, magnesium, iron, potassium, zinc, and even heavy metals. This binding process is why oxalates contribute to mineral imbalances leading to kidney stones and potentially leading to kidney disease.
Oxalates, when free and unbound, can create immense tissue damage throughout the body.
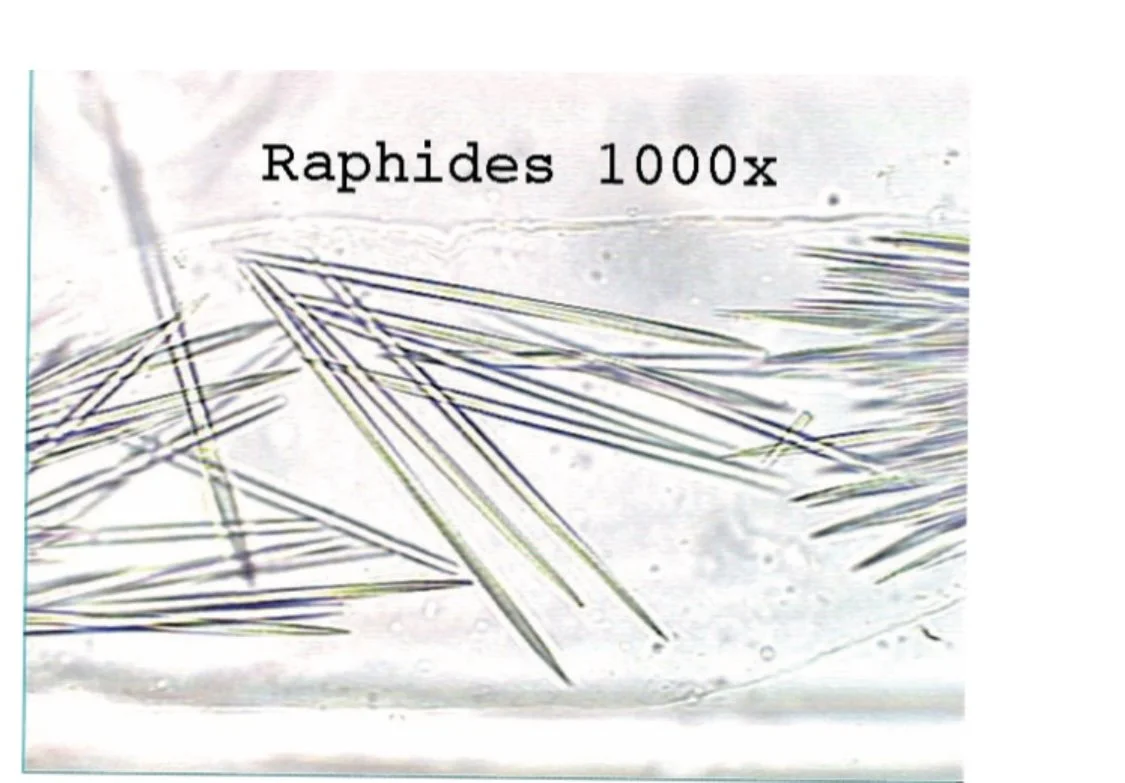
Imagine these very sharp needle-like oxalate crystals moving though your GI tract, blood vessels, kidneys, heart, and thyroid creating oxidative damage along the way.
1.1. History of Oxalates in the Human Diet
Oxalates are found in plant foods and were identified in 1769. Historically, plant foods high in oxalates were consumed seasonally and minimally. High oxalate foods were also consumed with dairy products or other foods which contained citrate minerals that would help bind to the oxalic acid and prevent human intestinal absorption.
For example, spinach historically was consumed with butter, cream or cheese which supplies calcium citrate to bind to the oxalates. Another example are the Andean highland’s Peruvian potatoes and their clay-based dipping sauces. ““The consumption of clay is ancestral," says Peruvian agronomist Alberto Salas. And, he says, clay may have allowed early inhabitants of the Andes to eat wild potatoes, which are toxic.”
Humans can safely consume 50-150mg of oxalates daily. Some people following the Standard American Diet are consuming up to 1500mg of oxalic acid daily! This overload of oxalic acid actually kills the beneficial microbes that help our bodies metabolize oxalates leading to intestinal and other organ damage.
Research on rats in 1939 demonstrated that oxalic acid is certainly an anti-nutrient and is also termed a plant toxin. We have known very clearly the diminishing absorption of calcium when oxalic acid is present in the diet since this 1939 article on the utilization of calcium from plant greens that contain high amounts of oxalic acid. Yet the widespread knowledge and utilization of these findings has greatly been ignored throughout the last 100 years.
1.2. Are oxalates bad for you?
Oxalates, in moderation, are not inherently harmful to most people. In fact, many foods that contain oxalates also provide valuable nutrients and health benefits. However, the key lies in maintaining a balanced diet and being mindful of the oxalate content in certain foods. For individuals with a history of kidney stones or certain medical conditions, managing oxalate intake may be crucial to prevent complications.
1.3. Why are oxalates bad for you?
Excessive oxalate consumption can lead to health issues due to the formation of oxalate crystals. These crystals can accumulate in various tissues and organs, increasing the risk of kidney stone development and other complications. When oxalates overload the system, they can hinder the absorption of essential minerals like calcium, contributing to a range of problems, including intestinal and organ damage.
The historical practice of consuming high oxalate foods with calcium-rich accompaniments highlights the traditional awareness of the need to balance oxalate intake for optimal health. Despite early research on oxalic acid as an anti-nutrient and plant toxin, widespread attention to these findings has been limited over the past century, potentially contributing to the increased oxalate levels observed in modern diets.
2. Oxalates in Food
Oxalates are naturally occurring compounds found in a variety of plant-based foods. These compounds can form crystals, leading to potential health issues, especially for those with a predisposition to kidney stones. Understanding the oxalate content in different foods is crucial for those who need to manage their intake due to health concerns.
2.1. Foods High in Oxalates
More and more “healthy” foods with high oxalates have been glorified and over consumed under the label “superfoods/nutritious”. Unfortunately, just because a food contains a nutrient like calcium, doesn’t always mean our bodies will be able to absorb that nutrient. Nutrition greatly depends on how the food is prepared.
Certain foods are particularly high in oxalates and should be consumed in moderation, especially by individuals prone to kidney stones or other oxalate-related issues. Leafy greens like spinach, nuts, berries, and certain spices such as cinnamon and turmeric are examples of foods with elevated oxalate levels. Being aware of these high-oxalate foods can help individuals make informed dietary choices to support their overall health.
So if you have been juicing beets and greens heavily (beets and greens), have been vegan for several years, or if you are consuming a lot of paleo baked goods, this article is for you.
2.2 Main food sources of oxalates in GAPS, AIP, or Paleo Diets:
In dietary frameworks like GAPS, AIP, or Paleo, which prioritize whole, unprocessed foods, oxalates become a notable consideration. Oxalate-rich foods are commonly included, such as nuts, seeds, and dark leafy greens. Balancing the nutritional benefits with oxalate intake is crucial to prevent potential health issues, making awareness of oxalate content essential for informed dietary choices within these protocols. Here are some foods that contain oxalates:
Almonds, cashews, chia, pine nuts, poppy seeds, sesame seeds, and most nuts/seeds (macadamia and pecans are the lowest in oxalates)
Beans and peas (gluten free grains and beans are very high in oxalates)
Blackberries and raspberries
Spinach and dark leafy greens (chard and curly kale are also high, while dinosaur flat leaf kale tends to be lower)
Beets/ beet greens
Okra
Plantains
Rhubarb
Cinnamon, turmeric, cumin, and ginger
Black tea and green tea
Sweet potatoes (AIP not GAPS)
Chocolate (Paleo not GAPS or AIP)
2.3. Is Honey High in Oxalates
While honey is generally low in oxalates, it's essential to note that the exact oxalate content can vary based on factors like floral source and processing methods. In most cases, honey is not a significant source of oxalates. However, individuals with specific dietary restrictions or health conditions may choose to monitor their overall oxalate intake, even from seemingly benign sources like honey.
2.4. Oxalates in Spinach
Spinach is notorious for its high levels of oxalates, which may cause complications for individuals at risk of oxalate-related issues, such as kidney stones. Despite its nutritional value, the oxalates in spinach can hinder the body from absorbing essential minerals and may negatively impact the balance of good bacteria in the gut. Those concerned about higher oxalate levels in their diet may need to limit spinach consumption or adopt specific preparation methods, like cooking, to reduce oxalate levels and mitigate potential health risks.
2.5. What Foods Neutralize Oxalates
Certain foods, particularly those rich in calcium and magnesium, may help mitigate the effects of oxalates by binding to them in the digestive tract. Dairy products, for example, can provide enough calcium, which binds to oxalates, reducing their absorption. This strategic approach is crucial for individuals looking to manage their oxalate intake effectively and support overall kidney health. By incorporating foods high in calcium into their diet, individuals can address concerns related to oxalate, oxalic acid, and calcium oxalate. This becomes particularly relevant in the context of kidney stones and low oxalate diets, where the balance of calcium and oxalate is essential. It's important to understand how calcium-rich foods contribute to preventing the formation of calcium oxalate stones and to be mindful of increasing your calcium through dietary sources or calcium supplements as a proactive measure for kidney health.
3. Symptoms of Oxalate Toxicity
Not everyone will experience symptoms of oxalate toxicity. These symptoms are dependent on genetics, how many oxalates are consumed, and the microbiome. Symptoms related to oxalate toxicity can be difficult to identify in light of the varied symptom expressions from person to person. It is important to be aware of ancestrally consistent recipes of oxalate foods since more and more of these foods are eaten in new ways that might increase the risk of oxalate toxicity. Listed below are potential symptoms related to oxalate toxicity:
Kidney stones/disease
Autoimmunity
Frequent urination
Headaches
Low every/general malaise
Sleep disorders
Autism (Autism and Oxalates)
Thyroid dysfunction (Hashimotos, Graves, generalized thyroid disease)
Arthritis/ joint pain / back pain
Chronic gut issues
Impaired bone health, neurological, cardiovascular, and kidney function
3.1. Lab Testing to Confirm Oxalates:
Oxalates can be confirmed using a urinalysis and an OATS test or Great Plains Organic Acids Test. However, lab testing can be hit or miss because the body is not constantly dumping oxalates.
3.2. Oxalate effects inside the cell:
Oxalates disrupt intracellular enzymes such as Pyruvate Kinase
Ex: Pyruvate Kinase is needed in the last step of the glycolysis process. When disrupted by oxalic acid, the body cannot properly metabolize carbohydrates into ATP. ATP stores become insufficient leading to chronic fatigue.
Oxalates affect cell membrane function
Phospholipids such as phosphatidylserine get dislodged from the cell membrane (affecting sleep and leading to “hit by a bus” feeling)
Oxalates enter the cell and ruptures liposomes and hydrolytic enzymes which spill out of the cell (leading to inflammation and oxidative damage)
3.3. Endogenous Oxalate toxicity (Oxalates created inside the body):
Some individuals who reduce their oxalate load may still experience oxalate symptoms. These individuals may overproduce their own oxalates through incomplete metabolic processes (i.e. Idiopathic Calcium Stone Disease), where glyoxal is converted to oxalate by glutathione and the glyoxalase systems.
This is rare but can occur in the following perfect storm:
Oxidative stress
B6 and B1 deficiency (some medications such as ___ deplete B6)
Excess glycine and hydroxyproline in the diet (too much bone broth instead of meat stock)
Specific medications which deplete B6
Increased vitamin C supplementation
4. The Role of Oxalates in Kidney Health
Oxalates play a crucial role in kidney health, especially in the formation of kidney stones. Excessive oxalate intake, often found in certain foods, can contribute to kidney stone development. Recognizing this connection is vital for individuals seeking to protect their kidney health and make informed dietary choices to manage oxalate intake and prevent the developing of kidney stones.
4.1. How Oxalates contribute to kidney stones?
Oxalates play a significant role in developing kidney stones. Calcium oxalate stones are a common type of kidney stones often develop due to the accumulation of oxalate crystals in the kidneys. The risk of kidney stones is heightened when individuals consume an excess of high-oxalate foods. Understanding the types of kidney stones and their formation mechanisms sheds light on the crucial relationship between oxalates and kidney health.
4.2. Managing Oxalate Intake for Kidney Health
Given the potential risks associated with oxalates, managing their intake becomes paramount for kidney health. Adopting a low oxalate diet is often recommended for individuals at increased risk of kidney stones. Identifying foods high in oxalates and incorporating cooking methods that reduce oxalate levels can contribute to a proactive approach in managing oxalate intake. This section delves into effective strategies for individuals to navigate their dietary choices, fostering kidney health and mitigating the impact of oxalates on stone formation.
5. How to Reduce Oxalate Toxicity
Mitigating oxalate toxicity is vital to prevent kidney stones and promote overall well-being. Here are a few actionable steps to successfully reduce oxalate levels:
Eat seasonally
When consuming foods with oxalates, consume with dairy and animal based calcium sources (1 cup sour cream = 250mg Ca; 1 cup yogurt= 450mg Ca; 3 oz sardines= 370 mg Ca) Dependance on Oxalate Absorption on the Daily Calcium Intake.
Oxalates are highly water soluble and can be reduced by boiling the high oxalate food and making sure to discard the water (e.g. Boil beets and discard the water).
Improve bile production by increasing digestive enzymes by consuming apple cider vinegar, TUDCA, or oxbile supplementation. Undigested fat binds to calcium rather than calcium binding to oxalates in our food which allows for more absorption of oxalates into the body.
Gut bacteria and oxalates: Two probiotics can help metabolize oxalic acid
Oxalobacter Formigenes
L. Gasseri (not good if you have histamine intolerance)
L. Planetarium (good for histamine clients and is mostly found in kefir and yogurt)
Antibiotics (i.e. z pack and azithromycin) kill these beneficial microbes but so does overconsumption of oxalates.
Reduce oxalates in the diet slowly. Reduce by 50mg each week to avoid severe oxalate dumping until you reach 50mg /day.
5.1. What is Oxalate Dumping?
Oxalate dumping is a term used to describe what happens when the body stops absorbing oxalates and starts eliminating the stored toxin. If there is a high oxalate load in the body, there will be a perceived safety to rid the body of oxalates when very little or no oxalates are absorbed. This process can be uncomfortable and present with the following symptoms.
Oxalate Dumping Symptoms
Keto rash
Watery or sandy stools, morning or after eating frequent
Burning stools
Pain in kidneys
Inflammation in the joints
Crusty eyes
Extreme fatigue, dizziness, headaches
Foamy, cloudy urine
Shooting pain in the jaw
Rapid acidity (acidosis)- more rare, but presents as odd breathing, for example, out of breath walking across the room
What causes oxalate dumping
Vitamin C
B complex vitamins
Fasting- excess dumping during a longer fast
A sudden drop in oxalate consumption
Creating healthier and stronger bodies- as the tissues get healthier, it will begin to dump more (i.e. random dumping several years into a healing protocol)
5.2. Rules To Support Oxalate Dumping:
For kidney pain, take D-mannose and magnesium citrate to support the urinary organ tissue during oxalate dumping
D-mannose 2g/day for oxalates
D-mannose 10g/day for UTI
1000mg of magnesium citrate
For diarrhea, calcium citrate 1-2g no more than 3000mg
Dairy 2-3 servings of butter, cheese, yogurt, or kefir daily.
For constipation, magnesium citrate to bowel tolerance (CALM drink)
For heart palpitations, potassium citrate 1-4g or 4-5000mg
Never use citric acid (ascorbic acid) if still consuming oxalates
You can still accumulate oxalates if you eat high amounts of oxalates. Reducing the intake of oxalates slowly and then taking calcium and magnesium citrates will aid in dumping stored oxalates.
5.3. How to flush oxalates:
Flushing oxalates from the body involves implementing various strategies aimed at promoting the elimination of excess oxalates and supporting overall health.
Here are key approaches to consider:
Stay Hydrated
Adequate hydration is crucial for promoting kidney function and facilitating the elimination of oxalates through urine. Drinking plenty of water helps dilute oxalates in the kidneys, reducing the risk of crystal formation and promoting their natural removal from the body.
Regular Exercise
Engaging in regular physical activity promotes overall kidney health and may contribute to the flushing out of oxalates. Exercise stimulates blood circulation and enhances kidney function, supporting the efficient elimination of waste products, including oxalates, through urine.
Consider Oxalate-Binding Agents
Certain substances, such as calcium citrate supplements, may act as oxalate-binding agents in the digestive tract. These agents can help prevent the absorption of oxalates, supporting their excretion from the body.
Consult with a Healthcare Professional
Individuals considering specific strategies to flush oxalates from the body should consult with a healthcare professional. A personalized approach, taking into account individual health conditions and dietary needs, can ensure the adoption of effective and safe methods for managing oxalate levels.